Abstract
Background: The Joint Outcome Study (JOS) was a randomized controlled trial showing that, in severe hemophilia A, prophylactic factor VIII every other day starting prior to age 30 months leads to better joint outcomes at age 6 years than enhanced episodic treatment with factor VIII for bleeding1. After conclusion of the JOS, all participants were encouraged to continue on, or to transition to, prophylaxis. Here we describe the results of the Joint Outcome Continuation Study (JOS-C), which followed the participants of the JOS to age 18 years.
Methods: All participants of the JOS were eligible for the JOS-C. MRIs of 6 index joints (right and left ankles, knees, and elbows), index joint physical exam scores using the Colorado Haemophilia Paediatric Joint Physical Examination Scale2 , estimates of joint bleeding episodes, and surgery information were collected. The primary endpoint, as in the initial JOS analysis, was evidence of hemophilia-related osteochondral joint damage on MRI, scored using the extended MRI scale3.
Results: Of the 65 previous participants of the JOS, 37 gave informed consent for the JOS-C study, including 18 initially randomized to prophylaxis prior to age 30 months ("early prophylaxis"), and 19 initially randomized to enhanced episodic treatment who started prophylaxis at a mean age of 7.5 years (median 6.1, range 2.7-17.1, "delayed prophylaxis"). All initially on prophylaxis in the JOS continued on prophylaxis through the JOS-C. One participant (early prophylaxis arm) failed to complete an MRI, and four others (2 early and 2 delayed prophylaxis) had their MRIs excluded for technical reasons. Four participants (3 early prophylaxis and 1 delayed prophylaxis) developed high titer inhibitors during or shortly after the JOS and were analyzed separately.
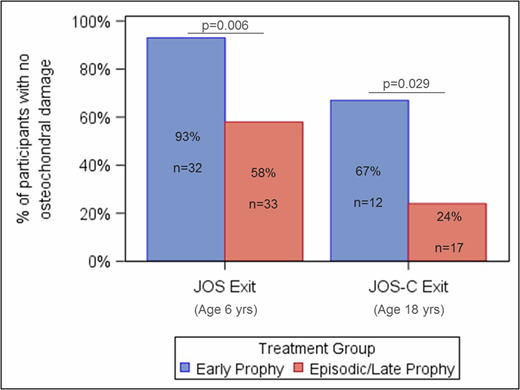
Osteochondral joint damage was defined as evidence of osteochondral damage on MRI or a need for joint surgery. The relative risk of osteochondral damage in those on delayed prophylaxis as compared to those on early prophylaxis was 6.5 (95% CI 1.3, 33.6; p=0.029). At age 18, 67% of those on early prophylaxis, and only 24% of those on delayed prophylaxis had zero index joints with osteochondral damage (Figure 1). Twenty-five percent of early prophylaxis and 47% of delayed prophylaxis participants had osteochondral damage to more than one joint. Most participants had some soft tissue changes on MRI, defined as effusion, synovial hypertrophy, or hemosiderin deposition. There was no difference in risk of soft tissue damage between initial treatment groups (p=0.48). Osteochondral damage scores were available for 3 patients with inhibitors: two with refractory inhibitors had osteochondral changes on at least one joint, and one with an inhibitor that tolerized within 3 months had no osteochondral damage. Total physical exam scores were also higher in the delayed prophylaxis arm (mean 22.6, standard deviation (SD) 15.5) than in the early prophylaxis arm (mean 16.2, SD 10.5), but this difference was not statistically significant (p=0.19).
Conclusion: The JOS-C demonstrates that, in severe hemophilia A, initiation of prophylaxis prior to age 30 months provides continued protection against joint damage throughout childhood. Those who started on prophylaxis later in childhood had higher risk of joint damage at age 18. Initiation of factor VIII prophylaxis in the toddler years is critical to preventing osteochondral joint damage and should not be delayed.
References
Manco-Johnson MJ, Abshire TC, Shapiro AD, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med. 2007;357(6):535-544.
Hacker MR, Funk SM, Manco-Johnson MJ. The Colorado Haemophilia Paediatric Joint Physical Examination Scale: normal values and interrater reliability. Haemophilia. 2007;13(1):71-78.
Hong W, Raunig D, Lundin B. SPINART study: validation of the extended magnetic resonance imaging scale for evaluation of joint status in adult patients with severe haemophilia A using baseline data. Haemophilia. 2016;22(6):e519-e526.
Figure 1: Percentage of participants with zero joints with osteochondral damage at JOS exit (age 6 years) and JOS-C exit (age 18 years), excluding participants with inhibitors.
Warren:Bayer Healthcare: Research Funding; HTRS/Novo Nordisk: Research Funding; Bayer Hemophilia Awards Program Fellowship Project Award: Research Funding; CSL Behring Heimburger Award: Research Funding. Shapiro:Genetech: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Prometic Life Sciences: Consultancy, Research Funding; Novo Nordisk: Membership on an entity's Board of Directors or advisory committees, Research Funding; Daiichi Sankyo: Research Funding; Kedrion Biopharma: Consultancy, Research Funding; Bio Products Laboratory: Consultancy; Bioverativ, a Sanofi Company: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bayer Healthcare: Other: International Network of Pediatric Hemophilia; Sangamo Biosciences: Consultancy; Octapharma: Research Funding; Shire: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; OPKO: Research Funding; BioMarin: Research Funding. Recht:Shire: Research Funding; Biogen: Research Funding; Novo Nordisk: Membership on an entity's Board of Directors or advisory committees, Research Funding; Kedrion: Membership on an entity's Board of Directors or advisory committees. Manco-Johnson:Bayer AG: Honoraria, Research Funding; Novo Nordisk: Honoraria; Biogentek: Honoraria; CSL Behring: Honoraria; Baxalta, now part of Shire: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal